 |
| Embolization |
What is Embolization?
Embolization is a minimally invasive medical procedure used to block one or
more blood vessels or vascular malformations. It is done by injecting special
medical materials called embolic agents into the blood vessel to reduce or
block blood flow to an abnormality. This is done through a small puncture in
the skin, most often in the groin or arm. The embolization material acts like a
miniature occlusion or blockage in the vessel. Once injected and settled in
place, it stops blood from flowing to that specific area. This blocks the blood
supply to an abnormality, such as a tumor or vascular malformation, inhibiting
its growth and potentially resolving medical issues.
How is Embolization Performed?
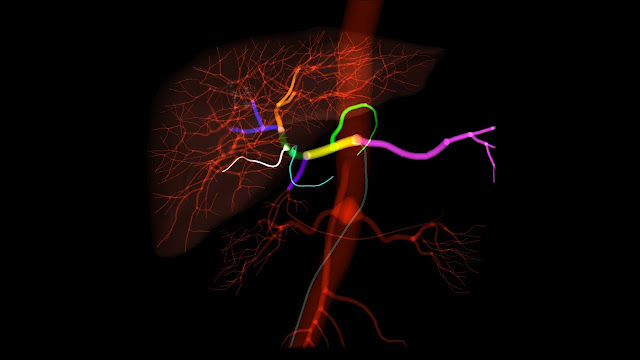
An embolization procedure begins with the patient undergoing an angiogram. In
this test, a catheter is inserted into the femoral or radial artery in the
groin or wrist. Using X-ray guidance, the catheter is threaded through the
blood vessels until it reaches the area of concern. A special dye is then
injected that makes the blood vessels visible under fluoroscopy, allowing
precise localization of the target.
Next, tiny embolic agents are prepared and loaded into a microcatheter. This is
a very small and flexible catheter that can navigate narrow blood vessels.
Under fluoroscopy, the microcatheter is carefully maneuvered into the feeding
blood vessel of the abnormality. The embolic agents are then slowly injected
through the microcatheter to restrict or stop blood flow to the problem area.
Types of embolization materials include gelatin sponges, coils, beads, and
glues.
After the materials are successfully placed, the microcatheter and angiography
catheter are removed. A small bandage is placed on the entry site. The patient
then goes to the recovery room for observation and is typically able to go home
the same or next day after confirming no complications. Follow-up imaging is
done to check for effective embolization.
Conditions Treated with Embolization
Uterine Fibroids: Non-cancerous tumors in the uterus that cause heavy bleeding,
pain, and pressure. Embolization
cuts off their blood supply, shrinks them over time, and controls symptoms in
many women.
Kidney Cancer: Used pre-operatively to shrink tumors, make surgery safer/easier.
Can also be curative if tumor thrombus in vena cava needs downsizing first.
Liver Cancer: Embolizes liver tumors to impede growth and spread. Palliative
treatment when surgical resection not possible to relieve pain, bleeding. Can
be used for chemoembolization.
Brain Aneurysms: Tiny sacs or bulges in blood vessels in the brain that can
rupture and cause a stroke. Embolization inserts coils to seal off the opening
and slow blood flow.
Varicose Veins: Abnormally dilated, twisted leg veins near the skin surface.
Occluding tributary veins with glue or coils redirects blood flow to deeper
veins.
Nosebleeds: Embolization ofethmoid arteries treats severe, recurrent nosebleeds
unresponsive to other measures by blocking arterial supply.
Arteriovenous Malformations (AVMs): Abnormal tangles of vessels that disrupt
normal blood flow. Embolization occludes these malformations to close them off
permanently or reduce size for safer resection.
Bone Cysts or Tumors: Precisely administered cement or other agents embolize
blood vessels feeding osseous lesions, hardening and shrinking them. Combined
with surgery as needed.
Gastrointestinal Bleeding: Embolizes culprit artery to stop active bleeding
from stomach ulcers, colon polyps/tumors, or other sources that cannot be
pinpointed by other tests.
Embolization Advantages
The chief advantages of embolization versus traditional open surgery include
being minimally invasive, less traumatic physically and psychologically for
patients, quicker recovery times, shorter hospital stays, reduced blood loss
and transfusions, avoidance of large incisions and general anesthesia, ability
to target very small distal vessels, and repeatability if needed. For some
conditions it provides definitive treatment without surgery. Embolization also
allows organ-preserving techniques over removal or resection. Overall it
provides safer, more cost-effective options for many medical issues previously
requiring open procedures.
Embolization Complications
As with any medical procedure, risks exist with embolization though they are
generally low. Potential complications include vessel perforation or dissection
during catheter work, infection at the entry site, reaction tocontrast dye,
organ/tissue injury from unintended embolization, and failure to fully occlude
the targeted blood vessels. Ischemic tissue death is possible if too much blood
flow is restricted. Complications are usually managed conservatively but
sometimes require intervention or open surgery. Close monitoring during and
after allows rapid treatment of any issues. With experience, complications
become even less frequent. Most patients recover problem-free after
embolization.
Future Directions
New embolic agents and advanced microcatheter technologies continue improving
embolization safety, precision, and effectiveness. Drug-eluting beads deliver
chemotherapy directly to tumors. Bioabsorbable materials avoid long-term vessel
occlusion concerns. Super-selective microcatheters access even the tiniest
vessels. Navigation is aided by computer-assisted fluoroscopy, 3D digital
subtraction angiography, and fusion with CT/MRI scans. Expanding clinical
applications include uterine fibroid treatment, endoleak embolization after
abdominal aortic aneurysm repair, trauma embolization, and numerous other
areas. Embolization remains a dynamic specialty at the forefront of minimally
invasive medicine. Its benefits will likely help many additional patients in
the years ahead.
By blocking targeted blood vessels through small catheter insertions, it
provides organ-sparing options over open surgery for conditions previously not
safely treatable without removal or resection. Continued advancements make
embolization an increasingly powerful tool for improving patient outcomes.
Get More Insights On This Topic: Embolization
